To comment on, or read comments on, a particular post, click on the post title.
- # 1 Introductionby Julie Bach
No one expects to become ill. Well, okay, I know lots of us harbor anxieties that we will end up with the diseases and conditions that seem to run in our families. Both my grandmothers had breast cancer, so in the back of my mind, wiggling about like a little worm, is a subcutaneous worry that I might end up with breast cancer too. But I’m guessing that most of us, if we’ve enjoyed nominally good health in the past, go about our days thinking that we’ll have decent health tomorrow too.
And then suddenly, perhaps because of an infection, or gradually, like the diminishing daylight in November, we find ourselves with a diagnosis. Even if a friend has warned us—Julie, if you keep going this way, you’re not going to see your kids through high school—we’re still shocked when a doctor tells us that we have a chronic illness that is difficult to diagnose and has no known cure. And then, six months later, we’re even more distraught when she tells us that, based on our blood work, that chronic condition is actually caused by another, underlying chronic condition with no known cure and about which little research is being done.* So we’ll just have to experiment with symptom relief for as long as it takes. Meanwhile, rest. Stop working (not that we’ve been able, for some time, to work at all). Accept help from others (but we are Midwestern! And German/Norwegian!).
And so, without any preparation, mental or physical, we find ourselves in the ranks of the chronically ill, and the world as we have known it, indeed our own bodies as we have known them, are whisked away into a past that suddenly seems more golden than it did when it was the present.
The disorders I’m dealing with are complicated and almost entirely unknown by the general public. Trying to explain them to family and friends is exhausting and discouraging. So, since writing, for me, requires less effort and brings greater satisfaction than talking, I’ve decided to share what I hope will be a healing journey here in this blog.
If you’ve happened upon this page, feel free to read future entries, or not read them. We live in a busy world; following a blog is a big ask, and it’s just not many people’s cup of tea. All I do ask is that if you respond in the Comments section, please be kind. Kindness is healing for all of us.
Good night, and joy be with you all.
Julie
*When I originally wrote this post, I was under the impression that ME/CFS is caused by Mast Cell Activation Syndrome (MCAS). I have since learned that MCAS is more likely a comorbid condition with ME/CFS.
- #2 What Is Mast Cell Activation Syndrome?by Julie Bach
If people were trees, I’d guess that one sapling in every forest has heard of mast cell activation syndrome. That’s most likely because fewer than one sapling in every forest has been diagnosed with the illness. But, according to the handful of medical researchers working on understanding the condition, there might be a pretty hefty stand of trees surrounding that one sapling that all have a mast cell disorder; they just don’t know it. MCAS manifests as such a strange variety of symptoms that it is usually misdiagnosed as two or three or even ten other concurrent illnesses. The limited number of patients who have been diagnosed might be the tip of a very unpleasant iceberg.
I was diagnosed first with chronic fatigue syndrome and then with MCAS. That makes sense, because it now appears that MCAS may be chronic fatigue’s daddy.* In fact, MCAS may have an entire brood of distressing progeny: fibromyalgia, multiple chemical sensitivities, POTS, irritable bowel syndrome, and much more. The common thread here is that all these conditions are of unknown origin and were first dismissed by medical science as hooey. It’s possible—and I stress possible, because a LOT more research is needed—that MCAS is the root (or a root) of all these branches. If science can figure out what causes MCAS and how to cure it, we may be on our way to curing a whole tree of suffering.
So, what is mast cell activation syndrome? Here’s the Sesame Street explanation (keeping in mind that I am myself a student of MCAS, not an expert):
Mast cells were our bodies’ first defense against cellular invaders. Apparently, for a time, they were our only defense. They were the army before we had the air force, navy, and marines. As such, they had to do all the work of defending our bodies. Eventually, our bodies developed a more sophisticated defense, or immune, system, with lots of players doing the work the mast cells had once done on their own. But the mast cells haven’t been put out to pasture—oh no. They’re still around and playing an important part in our bodies’ defense system. Unfortunately, in some people, the mast cells are working way too hard. Maybe they didn’t get the message that they’ve got plenty of help now? They are not standing down at all, ever, and are firing on the very things they are meant to protect. They are overly activated, hence the name mast cell activation syndrome.
Mast cells originate in the bone marrow and then spread throughout every type of tissue in the body. They’re not numerous, but they do tend to concentrate where the body interacts with its environment—the skin, the digestive system, and the respiratory system. So symptoms of mast cell activation can include itching, flushing, rashes, hives, wheezing, sneezing, difficulty breathing, anxiety, panic attacks, low blood pressure, rapid or racing heart rate, gastrointestinal distresses of all types, sleep disturbances, and . . . yep . . . debilitating fatigue.
There’s so much to explain about MCAS. As I learn more, I’ll try to pass it along.
Julie
My primary sources for this post are both from Lawrence B. Afrin, M.D. One of his presentations is available on YouTube as Mast Cell 101, and his book, Never Bet Against Occam: Mast Cell Disease and the Modern Epidemics of Chronic Illness and Medical Complexity (Sisters Media, 2016) is widely available.
*When I originally wrote this post, I was under the impression that ME/CFS is caused by Mast Cell Activation Syndrome (MCAS). I have since learned that MCAS may more likely be a comorbid condition with ME/CFS. Or not. At this point, nobody really knows.
- # 3 What’s the Plan for Today?by Julie Bach
This morning, my husband asked me my plan for today.

My reply: I have no idea.
It’s been a long time since I made plans for a day. Instead, I have hopes. Today, I hoped to do some grocery shopping and cooking, tidy up the kitchen, and plant the impatiens I bought yesterday. I truly thought it was a realistic list.
I was out of bed just before ten, had a cup of tea, blended my breakfast protein smoothie, and talked for a while on the phone with my sister and my mom. After I hung up, I thought a brief lie-down would be a good idea. Pacing is so important when you have fatigue. If you take the breaks you need, you can last longer.
I laid down at 11:30 a.m. thinking I’d need just twenty minutes of rest, but I fell asleep. When I woke, I was the opposite of refreshed and ready to go. Fatigue lay on top of me like fathoms of water. I turned just my head to look at the clock and felt the slump of disappointment that is so familiar these days. It was four o’clock in the afternoon.
I thought about the grocery store and the cooking and the kitchen and the impatiens. I kept thinking about them while I laid in bed, under the weight of an ocean, until about five o’clock when thirst and hunger pushed me down the stairs. I thought about them again when I’d had something to drink and eat. I could still get to the store. I could still plant flowers. Plenty of daylight left. But my arms and legs were weak strangers to me. They carried me up the stairs back to my bed, and that’s where I have remained.
Discouragement is the constant companion to chronic fatigue. It can pull you under and anchor you to depths you hadn’t known existed.
As much as I can, on days like today, I surface toward encouragements. In Pema Chodron’s When Things Fall Apart: Heart Advice for Difficult Times (Shambala, 1997), she writes, “We don’t know anything. We call something bad; we call it good. But really we just don’t know” (9).
I want to label the disassembling of today’s hope list bad. Negative. Disappointing. HopeLESS. Seems to me that it is all of those things. But Chodron may be right. I possibly don’t know anything. I possibly don’t know that there is some purpose to illness, some undiscovered sea creature of energy in the drowning of fatigue. So I don’t plan. I hope.
Hoping seems more in keeping with not knowing than planning does. So tomorrow, I’ll have a new hope list.
Julie
Photo by Julie Blake Edison on Unsplash
- #4 What Is Chronic Fatigue Syndrome?by Julie Bach
It must seem like a name that could apply to almost every American adult: chronic fatigue, aka always tired. Aren’t most of us working too many hours, called on to care for too many people or causes, and sleeping far too little? Don’t too many of us need caffeine to get going in the morning and a sleep aid before bed at night?
Yes, we are, to a large extent, a nation of people in need of not just rest but an intimate knowledge of how to rest.
But chronic fatigue syndrome, as doctors know it, is something else altogether. Many prefer that it be called myalgic encephalomyletis (ME), but honestly, who can even pronounce that name, let alone have a sense of what it means? (In the medical literature and online, the condition often goes by the acronym ME/CFS.)
The fatigue of chronic fatigue syndrome is something entirely other than the tiredness or exhaustion that most of us feel when we’ve, say, worked too many long days in a row, or had a few nights of poor sleep, or labored in the yard on Saturday and now on Sunday need a long afternoon nap.
The fatigue of CFS feels like someone has drilled holes in the bottoms of your feet and drained out all your blood. It’s feeling, when you wake from twelve hours of sleep (yes, twelve), that you have just finished a long day and need twelve hours more.
The U.S. Centers for Disease Control stipulates three conditions that must be present for a diagnosis of chronic fatigue syndrome:
- Greatly lowered ability to do activities that were usual before the illness. This drop in activity level must last six months or longer.
- Post-exertional malaise, or a worsening of symptoms after physical or mental activity.
- Sleep problems.
Other symptoms include problems with thinking or memory (brain fog) and worsening of symptoms while sitting or standing upright.
Check, check, check, check, and check.
The weird ones to me are the post-exertional malaise and the worsening of symptoms while standing up. I can tell you that there are moments in almost every day when I must lie down. This reminds me of the way hunger would hit with a vengeance when I was pregnant. One minute I’d be fine, and then the next minute I had to eat. Now. And just as with pregnancy hunger I needed a full meal, not a few crackers, with CFS the need to lie down can’t be satisfied by just sitting down. My body has to be horizontal. This symptom, perhaps more than any other, keeps me house bound. There’s no convenient place to lie down on a protest march or a walk through a museum or a hike by the river.
Post-exertional malaise is the other funky one. A long walk on a pleasant day is like a bank withdrawal that puts your account in the red. There’s no way not to pay up, which, in the case of chronic fatigue, means spending the next day in bed.
The worst part of all of this is its effect on my family. I know what it’s like to go through adolescence and into young adulthood with a parent who is often in bed. It’s not right. It gives one a shaky feeling about the world out there, and the world in here. I hope my children know that I would give every possession I have, every possession I will ever have, every past, present, and future reward or pleasure, to change this.
- #5 Crosbyby Julie Bach
To be out of step with the world and in step with a dog is a singular experience.
It is a quiet, secret existence known only to your non-judging companion. Only he observes all the mornings you can’t get out of bed until almost noon and all the afternoon hours you give up the quest for normalcy and lie back down. Your human family sees some of these mornings and some of these afternoons, but they, mercifully, are spared many of them because they are working or traveling or playing, as they should be.
Only the clear-eyed dog lifts his head every time he hears you crying for the life you’ve lost, and only his rough tongue licks your face every time you seek his thick, auburn fur for comfort. He’s the one who knows that, on good days, you hum when you walk, and on bad days, you don’t. In his soul are recorded your ups and downs, your prayers, your tantrums, your efforts to scrape yourself off the bed and into the world. His is a perspective that will remain forever unshared.
He died a week ago, and everything is empty: the bed, the rugs, the yard, the back porch. My face is empty. My hours are empty. The world’s observations of my life through his eyes are shut down.
Though I have tried in this blog to render a full picture of a life reined in by fatigue, no one—not one other creature—can know the outlines, shades, and contours of that life as he did. It does not matter that he could not speak to me in English of my experiences.
I spoke to him.
The silence of his absence is felt in the bones.

- #6 All Kinds of Tiredby Julie Bach
The truth is, there are all kinds of tired.
There’s the tired women feel when yet another man gets a promotion he doesn’t deserve or mansplains the obvious or sexually harasses herself or her friends.
There’s the tired black folks feel (I have not this experience, but I have ears to hear) when the knee on their necks doesn’t let up for one goddamn minute.
There’s the tired a father feels from working one sixty-hour week after another all the while watching corporate interests eat up his earnings.
There’s the tired of shopping, shopping, shopping and then buying containers and baskets and bins and ending up with the same unhappiness you started with, only now it’s accessorized.
There’s the tired of chemotherapy and the tired of addiction and the tired of feeling anxious or depressed all the time about nothing you can name. There’s the tired of not having enough and the tired of having too much, and the tired of not getting the one thing you’ve ever truly wanted.
There’s the tired of fearing that in this wealth gap, in this democracy under siege, in this rapidly changing climate, you will not be able to realize even the smallest of your life’s ambitions.
Everybody knows some kind of tired.
For me, chronic fatigue has made tired not just a personal experience but a social construct. I see it everywhere. Women and men, some with children, panhandling at intersections look so tired. Jamila Lyiscott, in her Ted Talk on having to code switch as a black woman, says, “I’m so tired of the negative images that are driving my people mad.” When Greta Thunberg said to world leaders at the 2019 U.N. climate action summit, “How dare you?” she seemed to me not only angry but exhausted. Tired of profits as usual, tired of the cowardice of the adults who are supposed to be managing the world for her future.
Many, many years ago when I first began taking notice of my health, a nutritionist said to a class full of women who were learning a new way to nourish themselves, “Most people just keep doing what they’re doing until they get tired of being tired.”
Are we tired enough yet?

- #7 The Self-Deceptionby Julie Bach
Before I stopped working completely, I took a semester’s leave of absence, hoping it would be enough to heal whatever was wrong with me and allow me to keep working. I wrote the following paragraphs sometime in the months leading up to that leave of absence.
The medical insurance representative on the phone says, “You take care now,” with genuine concern in her voice, and I start to cry. I’ve called to ask about coverage for the adrenal lab test I’ll be taking over the weekend. On Sunday, I’ll be filling four small test tubes with my saliva at points throughout the day, and then sending the lot off to a lab Monday morning. The test will measure my cortisol levels and thus the functioning of my adrenal glands.
The phone representative sounds worried, and I wonder if she knows something about this test I don’t. But I don’t let myself cry long. I have to call my primary care provider. The instructions she’s given me for the lab don’t match those on the forms that accompany the kit.
I pick up the phone in my office at the university and dial another number. I am overwhelmed with the extent of my fatigue. Since my late arrival at work this morning, I have done nothing but try and fail: try and fail to reply to emails, try and fail to work on program assessment. I am so grateful to have no students on my calendar today. I want—I want only—to drive home and crawl into bed.
I have been hiding this fatigue as best I can for a while now. After these phone calls, when I step out of my office, I’ll have a smile on my face and a cheerful word for my coworkers. After a conversation with a colleague in her office, a trip upstairs to consult with a librarian, and a moment with my writing tutors to provide some instructions, I’ll come back to my office, close the door, and sit, trying and failing for another hour to do any meaningful work. I don’t think clearly about the fact that it shouldn’t be difficult for me to type an email. It is difficult; I’m upset that it’s difficult; but I don’t ask why it’s difficult. I fear the answer. It’s easier to think of this day as an anomaly. A gosh-I’m-tired-today sort of day. Somehow my mind can strip from the thought of this day all thought of every other day that has been exactly like this one. It’s a neat trick, like taking a wide blade of grass and peeling it lengthwise into thin strands. Once the strands are scattered on the ground, none of them know about the others. The whole is lost.
In this way, I avoid the whole of my life. I keep up appearances to others. I keep up appearances to myself. The eyes that follow me when I walk in late, the increasing reliance on excuses, the weakness I feel when I step out of the house in the morning . . . they are merely shadows behind trees. They might contain something, but surely they are just shadows. When the sun shifts round to its position in the afternoon sky, surely I’ll see that there is nothing there.
- #8 Down By the Riverside, Part Iby Julie Bach
Gonna lay down my burden
Down by the riverside . . .
And study war no more.
I’ve been living with chronic fatigue syndrome for a long time, well before I was officially diagnosed. For years, I managed to deal with it, until I no longer could.
I know my doctor was relieved when I finally consented to take a leave of absence from work, and though she never said so, she was probably doubly relieved when my position was “eliminated.”
I’ve been out of work for five semesters now. It has taken me this long to grasp the lengthy menu of ways I keep myself plugged in to activities, in spite of the lasting costs to my health.
Chronic Fatigue and Long COVID
This awareness has come about recently largely because of media coverage of an illness being dubbed “long COVID.” You’ve probably heard of it: People who have COVID-19 are suffering months later from debilitating fatigue, brain fog, joint pain, and other symptoms. The resemblance of long COVID to chronic fatigue syndrome (ME/CFS) is striking. In fact, as the Harvard Medical School blog reported last fall, Dr. Anthony Fauci said that long COVID might be “the same as or very similar to” chronic fatigue.
In a fascinating read in a recent issue of The Atlantic, author Meghan O’Rourke points out the similarities between long COVID and conditions like ME/CFS, PoTS (postural tachycardia syndrome), and dysautonomia. O’Rourke (who herself suffers from a chronic illness and has been treated for Lyme disease) writes, “These are all poorly understood conditions that, evidence suggests, can be triggered by the body’s response to infections, with clusters of system-roaming symptoms that get grouped under one name.”
The attention on long COVID has been so great that even the PBS Newshour ran a beautiful and informative segment on ME/CFS from a patient’s point of view. It’s four minutes long and one of the best concise summaries of the history and impacts of the condition I’ve seen.
Post-Exertional Malaise
In all the articles I’ve read recently on these chronic conditions, one thing has bored a hole into my mind and won’t go away: the absolute necessity for patients to never exceed what some call their “energy envelope.”
One of the distinctive features of ME/CFS (and this may turn out to be true of long COVID as well) is post-exertional malaise, defined as “the worsening of symptoms following even minor physical or mental exertion, with symptoms typically worsening 12 to 48 hours after activity and lasting for days or even weeks” (CDC). Ron Davis, a Stanford scientist who has dedicated his career to finding a cure for ME/CFS, warns against ever letting oneself experience it. In an interview for CNN Health, he advises, “Know when you’re at your energy envelope limit. And don’t ever exceed it for any reason. Be serious about it.” He and the CDC suggest that “crashing” may prolong illness.
There’s no denying that for the past two-plus years I’ve been on a roller coaster of over-exertion and post-exertional malaise, an insane trip of over-do, crash; over-do, crash; over-do, crash. Like folks say, how’s that working for ya’?
Davis, in his interview, quotes an ME/CFS patient who suffered from the condition for five years and told him, finally, “I just got fanatical about it and decided I must never exceed my energy envelope. After a year of never crashing, I got over it.”
I have decided to do the same. I’m going to lay down my burdens by the riverside and stop warring with my beleaguered body. No more over-exerting. No more crashing.
I may have to give up a lot for a while, but every energy dollar I “bank” now may someday give me a fortune.
P.S. Thanks to Steve Johnson for the “banking” metaphor and for sending me the Atlantic article. Love you, Steve!
P.P.S. If you want to listen to a happy-fun rendition of “Down By the Riverside” featuring Louis Armstrong, click here.
- #9 Down By the Riverside, Part IIby Julie Bach
Turns out, resting is a difficult and perplexing pursuit.
We think we want to rest—I know I need to rest—but what we really want is to feel well rested. Then we can do the things we enjoy. Resting is a means to an end, not an end in itself. Resting is a pause in activities of value that enables us to do the activities of value. We say, oh how beautifully she dances or what a great cook he is, but we never say, oh how expertly she rests. Surely no one is admired for being good at resting.
And how would one be good at resting, anyway? Is there a competitive scale by which one could be judged? Points for duration, for resisting distractions, for resting prone instead of sitting upright, for keeping one’s eyes closed?
Years ago, Utne Reader magazine published an issue titled “In Praise of Idleness.” I was persuaded that idleness is a worthy enterprise. But idleness is not resting. Idleness suggests a relaxed state in which one is free to pursue whatever leisure activity comes to mind: sitting on the banks of a river contemplating the flowing water, lying in a hammock reading a book, sitting at a piano plucking at the keys (but not “practicing”). These scenes suggest a quiet engagement with the world, slow and relaxed, but an engagement nonetheless.
To rest, on the other hand, is to disengage with the world, to step out of the flow of time and human connection. An important and perhaps even life-extending disengagement if undertaken once in a while, perhaps even regularly, like a Sabbath, but believe me, a total bore when it forms your days for months on end.
Resting for me, so far, has meant lying flat on my back in bed staring at ceiling tiles. Or lying on my side noticing for the zillionth time that one of the knobs on my dresser is a shade whiter than the others. Sometimes it means listening to Madeleine Peyroux on Spotify; sometimes it means listening to no sound at all, except for the sounds I can’t stop—one neighbor’s barking terrier, another neighbor’s weed wacker. Sometimes, if I’m lucky, it will mean reading, but not for very long, because my brain tires as quickly as my body. Too much of the time it means scrolling through YouTube for a ticket to any mindplace but here.
In Part I of this post, I stated my intention to rest sufficiently to heal myself of chronic fatigue syndrome. To never crash, not once, to bank loads of energy dollars and never let my account fall into the red.
I am not looking forward to this.
I fear loneliness and boredom. I fear an empty mind and empty hands. I fear losing friends and missing out on the making of memories. I fear the deterioration of basic skills, like carrying on a conversation, navigating a shopping center, embracing a novel experience. I fear becoming old and strange and unknowable.
Could resting possibly be something else than it has been so far?
- #10 If I Keep On Hidingby Julie Bach
There’s a conundrum in writing about a chronic illness: tell the whole truth and you sound pathetic; keep the sad details to yourself and you’re not telling the truth.
The truth of a chronic illness like CFS or fibromyalgia or long covid is, well, yes, pathetic, both in the sense of arousing pity and in the sense of miserably inadequate (the two definitions offered by Google).
Neither sense is appealing for the person who considers sharing full descriptions of a chronic illness. So why bother?
I’m not sure why I feel a need to describe chronic fatigue syndrome, or why for the past year and a half I’ve hesitated so completely to do so that I haven’t published a single post on this blog. For one thing, I haven’t rested as I said I would, I haven’t stayed within that energy envelope (which, as it turns out, fluctuates wildly), and I’m not any better than I was a year and a half ago. I feel embarrassed, a failure. When I look at the day-to-day realities of my life, I see them as pathetic in Google’s second sense—miserably inadequate—and I fear that others will see them in the first sense—worthy of only pity. I do not want to be pitied.
I do, however, want to be known.
I listen to The Secret Sisters sing “If I keep on hiding, how will I be known / I keep telling myself that I’m better alone”* and I know that voice is mine. It’s easy to stay silent, hard to write, easy to avoid, hard to engage, easy to hide, hard to risk pity in the hope it might turn out to be love.

Image by Annie Spratt from Pixabay
* The Secret Sisters, You Don’t Own Me Anymore, New West Records, June 2017.
- #11 The Slow Process of Accepting Lossby Julie Bach
Have you ever noticed how films often use just one scene to show a character accepting a great loss? The character has an enormous cry in which all their grief pours down their face in tears and snot. Outside, thunder rumbles and rain beats down. In agony, the character falls to the ground after, perhaps, breaking something valuable, a metaphor for their former selves. Cut to the next scene: The character is shown leaving a house or entering some other building, with purpose, with confidence. They are a vessel emptied and refilled. The action of the film can now lead to its conclusion.
I have not found loss to be like that at all.
I cry in little bits. I pour off a tiny portion of whatever was in the vessel—my former me, former relationships, former goals—and for a while, maybe a long while, I just have less in the vessel. Less of a self. I’m four ounces of wine in a six-ounce glass; a pint of milk in a quart bottle.
In time, something I read or something someone says or something I experience adds a dram to the bottle. A bit of new wine, maybe better quality. A spoonful of fresher milk. I’m, say, sixty percent the old me and ten percent the new me. Still kinda empty.
After a while, I do a little more crying. I empty, am aware of the lack of me, and then fill a wee bit more. Now I’m fifty parts old and twenty parts new.
And so, over time that stretches as far as hope is from despair, I reckon with losses.
I should probably spend more time on this loss and transition process than I do. I could meditate, read, walk in the woods, write in a journal. But I’ll tell you, I am really resisting this emptying and filling business. The truth is, as much as I complained about the details of my life before chronic illness, I liked a lot of the basic contours. I. want. to. keep. them.
I want to keep my career, and specifically my most recent job. I want to keep my colleagues and my mentors and my students. I want to keep my involvement in my children’s lives, my visits to family, my time with friends. I want to travel more than I did, not less.
I’m very reluctant to let go of the old and extremely uncertain about the new stuff I’m putting in the bottle, or whether there even is anything to put in the bottle.
But I think it must be done. And maybe moving into the new, with courage, means crying in bigger bits, letting go of larger amounts at a time, sitting still for longer, and filling with greater amounts of quiet and unanticipated new.
After quite a few years of illness, I think I know how to do that. And I think I shall.

Photo by Zoe on Unsplash - #12 A Typical Dayby Julie Bach
On this typical ME/CFS day, so much like all the other days, I’m pleased to be out of bed at ten. That gives me a couple hours to rev up before the clock flips over into p.m. Something about waking after the stroke of noon feels like a defeat.
I put the kettle on and sit in the sunroom while it comes to a boil. I add a teabag to the pot and sit in the sunroom while it steeps. Then I pour myself a cup and sit in the sunroom for a very long while. I’ve gone from bed to sitting. This is progress.
I watch birds at the feeder. I read the morning news on my phone. I write up a list of tasks to do today. But mostly I’m tuning in to my body, waiting for a quiet signal that I have enough energy to start my day, hours after the rest of the world has started theirs.
Today the signal comes when I have been sitting for just an hour. I am so happy! This is good!
I dress, put in my contacts, and have a bit of breakfast. I feel remarkably clear-headed.
Up in my office, I open my laptop. I schedule an appointment with a new primary care physician (this has been on my to-do list for months). I message a question to the doctor who manages my chronic fatigue. I pay a bill online. I check my calendar for upcoming appointments. I’m worried because, two weeks from now, I have a medical appointment and a haircut on successive days. No time to recover in between. But the thought of not being able to go to two appointments in two days is still ridiculous to me. I close my calendar.
By now, fatigue is starting to make itself known. Just a little bit. It’s tapping me on the shoulder, not aggressive, but certainly insistent. I understand that I should lie down for a few minutes, take a “planned rest,” as one CFS expert calls it.
After ten minutes of lying flat on my bed, I’m impatient. I do have the energy to work, and I’m going to. Planned rests be damned.
Back to the laptop. I open a spreadsheet I’ve been building to track our charitable contributions. I make a phone call to one of the charities. Send an email to another. Peruse the spreadsheet and make some adjustments in formatting. But the fatigue of sitting at my desk really is catching up to me. However, I so much do not want to lie down. I’m sick of lying down. Maybe I can get up and move instead.
I tidy up my office. I make my bed and pick up clothes off the floor in the bedroom. I walk downstairs to get a glass of water in the kitchen.
But now fatigue is shaking me by the elbow. It’s poking me in the ribs, kicking the backs of my knees. I am so annoyed, so discouraged. But when I lie down on my bed and pull an afghan over me, I can’t deny the sheer physical relief.
I bring up Spotify on my phone. Click on the Wailing Jenny’s radio. I’ll take that twenty minutes planned rest and then I’ll drive to the neighborhood grocery. I know I can’t do a big shopping today, but I can pick up a few things to keep me going.
I wake two hours late. It’s gone four. Fatigue has simply moved in on top of me, pinning me to the bed. The trip for groceries fades away. Finishing the spreadsheet fades away. The possibility of cooking a good dinner fades away. Whatever “energy dollars” I started the day with are gone. I’ll lie in bed for an hour waiting to feel enough strength to get up. I’ll slap together a pb and j sandwich, talk for a bit with my husband, and go back to bed. This scenario has happened so many times that I don’t even really feel the disappointment. It’s muted, like the gray March skies outside.
But I loved my morning! I loved those hours in my office—doing, making, moving pieces of my life forward with skill and intelligence.
This has been a good day.
- #13 What Is Lost and What Is Foundby Julie Bach
A fundamental question for me in this blog is: How much do I rely on the tools of literature—story, character, image, lyricism—and how much on scientific objectivity? I know it’s not one or the other, but what is the balance?
We’re getting more scientific data about ME/CFS these days. Thanks largely to the attention paid to long covid, we have a better gauge of the number of people living with post-viral illnesses, what their symptoms are, and what treatments have worked, at least for some. We know a bit more about some of the biomechanisms of these illnesses, maybe a bit more about what’s happening at the cellular level.
But only through the details of story can I attempt to capture what living with relentless fatigue and post-exertional crashes is.
How do I communicate what is lost and what is found? How what is lost is the size of Lake Michigan, and what is found is the size of the pond at my cousins’ rural Michigan home when we were kids. We skated on the pond in winter, and in the summer, two pulls on a set of oars would row us out to the center of the pond, where we could slide overboard and swim without getting tangled in the weeds that filled most of the water.
On those visits to my cousins, would I rather have had the endless soft sand beaches, the wide sky, and the thrilling waves of Lake Michigan? Yes, I would.
But with my cousins, there was joking and laughter and a lot of sunshine, and all the kids and grownups eating burgers and potato salad afterward up at the house.
So it wasn’t Lake Michigan, but it lives in the memory as good.
- #14 What Do I Need?by Julie Bach
The light from a gray day in northwest Wisconsin is fading. Through the window in the cabin bedroom, the color is deepening from one adjacent Pantone shade to another, like someone is flipping through a color wheel. Soon I’ll see the reflection of what’s in the room rather than the trunks of the trees outside it.

I’ve been in bed all day. My energy bank account is at zero. Actually, it’s less than zero. I’m in debt. I’ve been reminding myself to take deep, slow breaths, and with each breath imagining a shiny quarter dropping with a plink into a piggy bank.
Earlier this afternoon, my husband stopped in the bedroom doorway and asked if I needed anything. After a moment, I shook my head, only because I couldn’t process his question quickly enough to give him an answer before he turned away.
If I had been able to think more quickly, what would I have answered?
Do I need anything?
Yes. I need someone to bring me a bowl of warm food that’s easy to swallow.
Do I need anything?
Yes. I need a friend or a family member or someone to ask me, how was today?
Do I need anything?
Yes. I need scientists to figure out the cause of this illness and discover a foolproof cure. I need them to have done that twenty years ago. I need all the doctors everywhere to be as educated about ME/CFS as they are about heart disease. Until they find a cure, I need all the doctors everywhere to have good ideas about how to manage this illness.
Do I need anything?
Yes. I need my friends to invite me to parties even if they’re probably right that I won’t be able to go. I need people to ring me up and tell me the latest news so I don’t feel so embarrassingly insignificant and out of the loop. I need my community to remember that I’m here and that I’m ill, even though they hardly ever see me and when they do I look fine.
Do I need anything?
Yes. I need the people from whom I’m asking these things to know that it’s truly okay that they don’t know what I need, because this illness is dismally uncharted territory for all of us. There’s no way they could know, and I do, truly, understand and accept that. But I need us to figure out what I need together, with no guilt, no blame, no recrimination, no apologies.
In short, I need what every human being on the planet—ill or well—needs: to be cherished as part of a loving community, and to be accompanied all our days.
Photo by zengxiao lin on Unsplash
- #15 O Gentle Sleep!by Julie Bach
You’d think someone who suffers fatigue would sleep like a baby, often and long. It is not so.
The cruel irony of ME/CFS is that sleep is as hard to come by, and as unpredictable, as love or fortune. Sleep can come easily by ten p.m. one night and hold off until three a.m. the next. It can hit at one in the afternoon, like a sudden, unforecasted snowstorm, last for five hours, and then stay away until dawn the next day. If it settles in at a normal time in the evening, it might very well stick around for the entire next day, while most folks are putting in a full day’s work.
Most of the time, sleep hangs around way too long in the morning, sometimes until noon. And then every so often, for no reason at all, it departs at daybreak and gives me what I almost never get: the hope of the rising sun and a full day of wakefulness.
Sleep is like the poor rabid dog in Old Yeller, zigzagging down the street at the end of the story with no control over its movements. Sometimes, I just want to shoot it.
As I understand it, sleep is like this for most people with ME/CFS. I’m not sure anyone truly understands why. (If you have an explanation, please share!) I believe one theory is that our autonomic nervous systems are awry, so the things our bodies would normally do without thought—sleep, digest, fight infections—they don’t do very well.
Of course, many older adults struggle with sleep. Such struggles are not uncommon. When I’m up in the night, even as late as two or three, I can see the light on over at my retired neighbors’. And I know my husband often wakes long before his six o’clock alarm, wishing his sleep had lasted longer. Nevertheless, I have the sense that, for the most part, adults my age are heading to bed some hours after the sun has set and are waking around the time the sun is rising, give or take. Whatever difficulties they may have with sleep occur within a basic regularity of sleep and wake cycles.
The only way to capture the difference between “normal” sleep and ME/CFS sleep is to picture it, so I created two charts.
The first is a chart of the hours I imagine a healthy adult sleeps and rests. Sleep is shown in blue, rest in purple. This adult gets into bed around ten on weeknights, reads for a while, and then falls asleep. On Friday and Saturday nights, she watches TV and skips reading. Watching TV that late may very well keep her awake, so she sleeps in a bit on Saturdays and Sundays and sometimes enjoys a rest on Sunday afternoons.
Normal Adult Sleep and Rest Chart
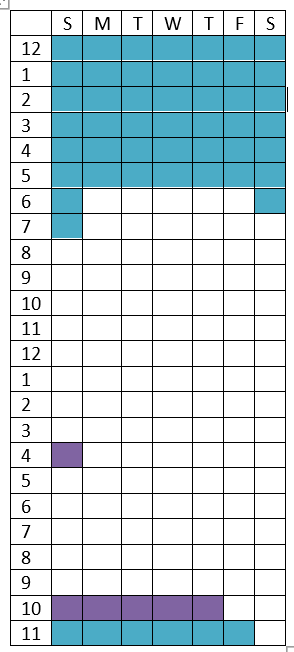
This is, of course, an imagined average, from which actual adults surely vary widely. My sisters, for example, are in bed by nine and up well before six every day, including weekends, and I doubt they’re getting a nap on Sundays. Some of my friends are night owls; they’re awake after midnight, productively engaged, and then rise later in the morning. The key, though, is that their patterns are fairly regular.
Now my own chart. Again, sleep in blue, rest in purple. And rest does really mean rest: lying in bed listening to music or a podcast or doing nothing. Watching TV and reading do not count as genuine rest for people with ME/CFS.
ME/CFS Sleep and Rest Chart
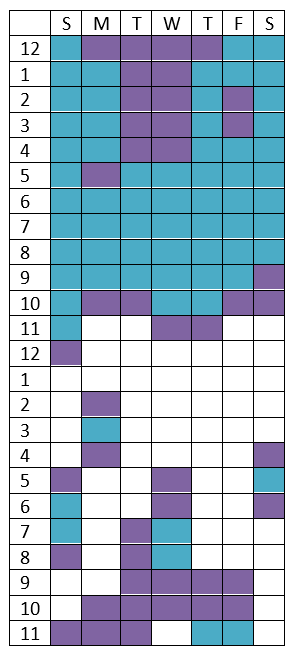
The most notable feature of my chart is the far fewer white squares. This is what I mean when I tell people (the few I do tell) that I have a limited supply of “energy dollars” to spend each day.
Having few energy dollars means that I will miss out on things and not accomplish much. But the really awful part of sleeping like this is the embarrassment.
One day last summer our ninety-year-old neighbor knocked on our back door shortly after eleven. I felt I had to answer because he might be in need of something, but I was in my pajamas and bathrobe. When I opened the door and he saw me, an awkward chortle escaped him. He looked down at the floor. I could only guess what he was thinking: Why is my neighbor in her night clothes in the middle of the day? My cheeks burned. (I haven’t explained my illness to this neighbor, nor to many others.)
To sleep in the middle of the day, when other adults are working, contributing to society, socializing, and just generally being adults, is to land in the realm of childhood—naps, and pjs, and lines on my face from the pillow at two in the afternoon. It’s not answering texts and not replying to emails and not picking up the phone. It’s eating a peanut butter sandwich for dinner because I wasn’t awake to prepare a meal. It’s incompetence squared.
When family or friends ask me what I was “up to” today, I never mention the hours of sleep and rest. “Oh, I haven’t been too busy,” is my evasive reply. I can’t imagine that there is anything to be gained by telling them I just woke up and am still in my pajamas.
And so the invisibility of ME/CFS continues. I perpetuate it by not being honest about the contours of my daily life.
Consider this my confession.
- #16 Something Is Not Rightby Julie Bach
I wrote this piece some years ago when I was still working. The fifty-year-old daughter of my mother’s best friend had died instantly of a sudden heart attack while out running with her dog. The dog stayed by her side on the snowy sidewalk until they were discovered.
The piece isn’t specifically about chronic fatigue syndrome, but I think it belongs in this blog for two reasons. One, the vast majority of ME/CFS patients are women. I hope both medical researchers and sociologists are looking into why that is the case. Two, the lack of exercise in my life now due to the risk of post-exertional malaise, combined with a family history of heart disease, does have me worried about my own cardiac health. Living with chronic fatigue syndrome has slowed me down immeasurably, but I know I still need to pay attention to the things that are not right.
All over the United States, women in their fifties and sixties are dropping. Into snow banks as they run their dogs, on the floors of their bedrooms as they rise from another poor night’s sleep, in the aisles of grocery stores between the boxed pastas and the canned vegetables. They have no time to clutch at the hearts that are ceasing to beat. They have no warning.
Except . . .
. . . the feeling on some days or over weeks or even months that something is not right. Not the same things that are always not right—the subordinate positions at work that don’t do justice to their skills and intelligence, the exhausting tensions between their husbands and sons, the hunger they feel all the time because lunch is never more than crackers and an apple. This is something different, something hard to touch. No chest pains. Maybe some heart palpitations. No pain in the upper left arm. Maybe an uncharacteristic headache. A touch of nausea. Catching themselves about to fall at the bottom of the stairs. Putting the kitchen sponge in the refrigerator.
And then, without any warning at all, they are gone. Their families are in shock. Their friends and coworkers protest, but she was so healthy!
What the friends and loved ones didn’t see was how many times a day these women paused, their fingers over their keyboards, and thought, why in hell do I have to reply to this email? How many times a day they pushed themselves up from their desks to solve another problem that was supposed to be someone else’s responsibility. How many times they hoped someone else would plan and cook the nourishing dinner they really needed. How many times they got in their cars and quick turned on the radio because if they left themselves any quiet in which to think they would come to conclusions their lives would not support.
Instead, they kept going—working, shopping, solving, caring—until that thing they couldn’t touch became their last hard truth.
